Call The Doctor
All About Stomach Cancer
Season 35 Episode 2 | 26m 59sVideo has Closed Captions
Learn risk factors, possible symptoms, how different types are found and treated
Stomach cancer, also known as gastric cancer, isn’t the most common cancer out there. But because it doesn’t always cause symptoms in its early stages, stomach cancer is often caught late. We’ll dive into risk factors, possible symptoms, how different types of stomach cancer are found and treated, and which other organs might have a connection.
Problems playing video? | Closed Captioning Feedback
Problems playing video? | Closed Captioning Feedback
Call The Doctor is a local public television program presented by WVIA
Call The Doctor
All About Stomach Cancer
Season 35 Episode 2 | 26m 59sVideo has Closed Captions
Stomach cancer, also known as gastric cancer, isn’t the most common cancer out there. But because it doesn’t always cause symptoms in its early stages, stomach cancer is often caught late. We’ll dive into risk factors, possible symptoms, how different types of stomach cancer are found and treated, and which other organs might have a connection.
Problems playing video? | Closed Captioning Feedback
How to Watch Call The Doctor
Call The Doctor is available to stream on pbs.org and the free PBS App, available on iPhone, Apple TV, Android TV, Android smartphones, Amazon Fire TV, Amazon Fire Tablet, Roku, Samsung Smart TV, and Vizio.
Providing Support for PBS.org
Learn Moreabout PBS online sponsorship(uplifting music) - [Narrator] The region's premier medical information program, "Call the Doctor".
- Stomach Cancer or gastric cancer is not one of the more commonly diagnosed cancers according to oncologists, but because it doesn't always cause symptoms in its early stages, cancer of the stomach is sometimes caught late.
We wanted to gather the best information for you about risk factors, which symptoms to take note of, and how different types of stomach cancer are found and treated.
All about stomach cancer in this episode of "Call the Doctor".
And, welcome to this episode of "Call the Doctor".
I'm Julie Sidoni.
Let's get right to tonight's panelists.
I'm really happy that we have three great physicians who have joined us tonight.
Dr. Ahmad Hanif, let's start with you.
And, thanks for being here.
- I'm very happy to be here.
My name is Ahmad Hanif.
I'm one of the medical oncologists at Geisinger Wyoming Valley Medical Center, and I treat patients with various type of cancers at Henry Cancer Center.
- Alright, great.
Thank you for being here, Dr. Oxenberg, Jacqueline Oxenberg, nice to have you back.
- Thank you.
Thank you.
It's great to be back.
I'm Jacqueline Oxenberg.
I'm a surgical oncologist also at Geisinger Wyoming Valley and I also treat a number of different types of cancers.
- And, Dr. Greenwald, - Yes.
- Thank you for being here.
- Thank you.
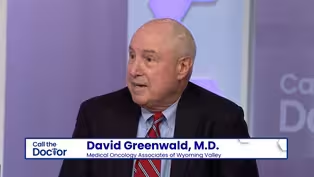
Dr. David Greenwald.
I'm in private practice with Dr. Bruce Seigman in Kingston, medical oncologists, and we see all types of cancer.
- Well, we welcome all of you.
I would like to start by defining stomach cancer, although I understand that's kind of a strange thing to say.
It seems to me there are different types of stomach cancer.
So, I'd like to start out by knowing a little bit more about what those different types are.
Do you wanna start there, Dr. Hanif?
- So, yes, absolutely.
So, gastric cancer or stomach cancer, it can be divided into various types based on the location or how it looks under the microscope.
So, based on the location, we know that the gastric cancer, the stomach cancer, and the cancer of the food pipe, esophageal cancers, they kind of overlap in the middle.
So, when we talk about stomach cancers, we start off right at the junction of the esophagus in the stomach, which we call gastro esophageal junction or GE junction.
So, the cancer over there is treated slightly differently than the cancer in the rest of the body, but the stomach has other parts of the body, the fundus, the main body, and the antrum, and the pylorus.
And, the cancer can be divided into different types based on where it's coming from.
But, when the cancer is examined under the microscope, then we see different types.
And, by far, the most common type that we see is a type called adenocarcinoma, which is a cancer that arises from the very inside lining of the stomach.
But, there are other types of cancer that arises from the stomach as well, like lymphomas, or sarcomas, or gastrointestinal stromal tumors.
- So, do they look different, Dr. Oxenberg, if you're looking for a type of stomach cancer?
Is... Can one be a tumor and one is a different look?
In layman's terms, what do you sometimes see?
- So, adenocarcinoma can present in two different ways.
One is the intestinal type can present as a mass inside of the stomach, but the intestinal type can present in the wall of the stomach.
And, sometimes we see that where the lining of the stomach doesn't look normal and the stomach just doesn't distend or open up like a balloon should when you eat.
Some of the other types of cancers are not the same.
They do present in the wall, but sometimes cause masses into the stomach as well.
- Is it typical, Dr. Greenwald, that if you see stomach cancer, you might also find it elsewhere or...
I mean, I know the stomach cancer is quite rare, but is it more likely to be found with other issues elsewhere in the body?
Can you tell me a little bit about how you typically see it?
- Well, unfortunately, and you may not...
This may not answer your question directly, but at least 50% of the time, it's advanced, so that it's found in other organs, it has spread from the stomach.
The most common area would be to the liver, but it can spread to lymph nodes in the abdomen, it can spread to the abdominal lining or the peritoneum.
It can spread to the ovary.
So, 50% of the time, it is spread at the time of diagnosis and, half of the other people, it will spread if it hasn't, or you find it spread when you do the evaluation prior to definitive surgery.
- More common that it started in the stomach and then spread or the other way around?
- More... Well, it starts... Stomach cancer by definition starts in the stomach.
But, as I say, it's silent for months if not years.
And, by the time patients develop symptoms, unfortunately 50% of the time, when you do the imaging when you do the evaluation, you find it elsewhere.
And, then surgeons like Dr. Oxenberg, before they would consider surgery, might look in the abdomen, just because they know it could be hiding there.
And, again, half of those people, another 25%, it's really spread outside the organ.
- You kind of segued right into something we were gonna talk about anyway, which is symptoms.
And, the reason I wanna get into symptoms is because I think these particular symptoms look and feel like a lot of other things.
So, could you, I guess we'll start here again.
What are some of the symptoms and do you see that they... Do they kind of look like many other illnesses?
- Yeah, so a common misconception is that the cancer is painful.
It's...
Most of the time it's not.
And, the symptoms could be very, very non-specific and very non-severe as I would say for years before they start making an impact on your life.
So, symptoms could be something like heartburn, or pain after eating, or an upset stomach, or bloating.
But, then other things could be noticed as well, like some people gradually start losing weight, or some people develop iron deficiency in their blood work, and that's usually a sign that something more sinister is going on than a... Just a simpler reflux disease.
- Is that partially why you think this is not diagnosed until very late, because it's a stomach ache and heartburn, and maybe people just work right through stomach ache and heartburn, Dr. Oxenberg?
- Yeah, I...
I think these are not symptoms that change overnight.
These are symptoms where people just slowly are not eating as much, they're not tolerating as much.
Depending on where the cancer is, sometimes the stomach actually narrows and, as you know, the rest of the stomach may actually distend and accommodate for those meals.
Yeah, so the symptoms are very vague and it often is picked up when it's too late because of that.
- Are there certain conditions that someone might have where you would think, I betcha...
I should monitor this person, I should watch this person at... - [David Greenwald] Well... - [Julie Sidoni] Yeah, go ahead.
- It's very common to have GI symptoms, whether it's reflux, ulcer disease.
Once you get into the system with a gastroenterologist who might be treating you, they often look in the stomach, and so there are things that they find, and then they keep a closer eye.
There's something called a Barrett's Esophagus when you're changing the lining of the lower esophagus because of constant reflux over years.
And, we know that that could be a precursor, that lining is more susceptible to developing a cancer.
If someone has an ulcer, and you do a biopsy, and you find a bacteria called H. pylori, those people have a higher risk of developing a cancer sometime in the future, not that everyone will, most won't, but at least those people need to be watched.
They're at higher risk.
But, I think the basic problem that you first mentioned is these are really common symptoms.
I mean, we all get indigestion, we all take Tums, we all have reflux.
And, so it's a tough call.
When do you say maybe something more serious is going on.
- So, I'm sure there's not one bullet point here, but is there a time, is there a range that you would give your patients, say if these symptoms go on for X, you really should give us a call?
- Well, sometimes your family doctor will prescribe a ulcer medication, a proton pump inhibitor, or a H2 inhibitor, and if, after two or three weeks, you're not really getting better, maybe that's the time to call and say, maybe I need to have someone look in my stomach.
- Right.
What about risk factors, not just conditions that you might see, but is there a lifestyle component or risk factors that you also see as a connection here, Dr. Oxenberg?
- Yeah, so smoking is definitely one of them.
Obesity is a large part of why we're seeing a shift in the types of gastric cancers to the lower esophagus, upper stomach, so overweight, obesity.
We also know genetics is part of this too.
While most patients that are... Or most people that are diagnosed with gastric cancer present later in life, sometimes there are some genetic mutations that can predispose patients to develop that much earlier in life.
- Let's talk about that for a few minutes.
The...
I'm sorry, genetic mutations.
Is there a time when you would say, earlier you said if someone has cancer, young stomach cancer, young, what is young?
What are you looking for in these genetic mutations?
- Unfortunately, I have to say sometimes we see patients in their 20s, 30s, early 40s with gastro cancer, and those are patients that I would definitely refer for genetic testing.
Sometimes, when they do the pathology and they look at the cancer themselves, they can actually determine if there's genetic alterations I'll say, as well, that may predispose people to having a genetic problem too.
- And, in that case, you would want them to speak with family members, et cetera.
- Yeah, yeah.
- We'll go back to the lifestyle risk factor type question if you have anything to add there, Dr. Hanif.
You said smoking and a couple of others.
Anything else come to mind for you?
- Yeah, so I mean some of the risk factors are general.
They're true for many different cancers.
Smoking being one of them, excessive alcohol drinking, less physical activity, being overweight.
These are true for many different cancers, including the stomach cancer.
And, then the risk factor specific for the stomach cancer would include infection, especially with the H. pylori bacterium and eating more salted or preserved foods.
So, those are the factors specifically for gastric cancer, but smoking is probably responsible for more stomach cancers than these factors in the present age.
Is that right?
- There is...
There has been a shift in the risk factors in the last decade or so.
So, we are getting a little bit better at treating H. pylori infection and people are eating less preserved foods and less salted foods.
So, we are seeing more and more of that cancer that comes on without H. pylori or without any history of eating too much preserved salted foods.
So,, that's been a change in the spectrum of the type of gastric cancer in the last couple of decades.
- Is there a screening for it?
- Currently, screening for an asymptomatic person, meaning a person who does not have any symptoms is not recommended, but screening based on symptoms is decided by the primary care provider and the gastroenterologist based on how risky they feel the overall symptomatology is.
- And, can you tell me about that screen?
What is it?
- So, most of the time the screening test is a test called endoscopy in which a camera is put down from the throat and they look inside the stomach, and if there's anything suspicious, then they take a biopsy.
But, for persistent symptoms, kind of what Dr. Greenwald alluded to, somebody who's reflux is not getting resolved after treatment with proton pump inhibitors or H2 blockers.
Other screening tests like detect...
Trying to detect H. pylori in the stool or in the breath, that can also be employed.
- That's...
I see you nodding over there.
- Well, a couple things.
One is people often, not confuse, but they put them on the same level, a colonoscopy and an upper endoscopy.
I'd like the audience to know that the upper endoscopy's really an easy procedure.
There is no prep, which is really the downside of a colonoscopy.
And, with conscious sedation, you don't even know that somebody's put a scope in your stomach.
So, it is a very simple procedure.
- Is it safe to say you do them often?
- As a patient, you can do it every week and not mind it.
Patients do not mind upper endoscopy.
So, I just want the public to know that.
- [Julie Sidoni] No, that's... - People fear colonies primarily because of the prep, but there is no prep for the upper endoscopy.
- I think people fear a lot of tests for various reasons.
Do you think that more people should be tested for this cancer?
- Well, it's easy for me to say that, but it's controlled to a certain extent by the insurance company and they have criteria.
Things have really changed though.
There was a time, probably up to about 1930 or 40, when stomach cancer was the number one cancer, number one cause of death in this country.
And, then it was in all the early textbooks, the incidence of stomach cancer, which is really the older diffuse type, the linitis plastica stiff stomach.
The incidence of that start going down every decade.
And, then unfortunately somewhere in about 1970, the cancer at the GE junction started to increase.
So, most of what we see today is really cancer of the lower esophagus, or the GE junction, or to the very proximal, the early part of the stomach.
And, that's different, the symptoms are different.
Usually, it's a swallowing problem, things get stuck, and so it...
The whole picture has changed.
We just fortunately don't see a lot of stomach cancer.
- I learned from all of you that it is the highest cancer deaths in certain other countries, Japan, Korea.
I didn't realize the incidence was so high there.
Why is that?
I mean, not that I expect you to know that...
I mean, why... Why is the... What's the thought there?
- When those populations come to America, their incidence of that disease falls and becomes like us.
So, it has something to do with their lifestyle in those countries.
I know that at one time there was an association with a liver fluke, clonorchis.
Their eating habits are different.
They eat a lot of uncooked fish and so forth.
- It could be a number of things.
- Yeah, I would not wanna stop eating sushi, but... - Right.
- But, it could be a lot of those things, but it's very high.
They actually do screening in those countries, 'cause it's so high.
- You were gonna say something, Dr. Oxenberg?
- I was just gonna say I think the liver fluke is the cholangiocarcinoma, which is still... - It was at one time stomach too.
- Let's talk a little bit about surgery and treatment.
This... Kind of getting it...
Throw the ball onto your court here, what... A patient comes to you with this, now what?
Are there different types of treatments and surgeries?
What's your rule?
- So, when I talk to patients, I break it up into three different groups when it comes to stomach.
And, I'll even talk a little bit about lower esophageal cancer too.
There's one group of patients, which they're very fortunate, it's a very early stage, sometimes if it's a very, very early stage, our gastroenterologist can actually remove that.
But, if it's at a very early stage and there's not very... Not much risk of spreading, I'll send them for a special scope with an ultrasound to see how far it is into the wall of the stomach, and if it's not high risk for spreading, sometimes they can go straight to surgery.
Unfortunately, the majority of patients fall into the second or third category.
The second category is where there is a risk of spread and that risk of spread is determined by the CAT scan.
If there's lymph nodes involved, determined by that scope.
And, if there is that risk of spread, that's when we're talking about doing what's called a laparoscopy.
Just a couple small incisions looking inside the belly, making sure that there's really nothing spread.
And, then doing multi-modality therapy, where we know that Dr. Hanif and Dr. Greenwald give the patients chemotherapy first followed by surgery, followed by chemotherapy.
And, that actually greatly impacts the survival.
Unfortunately, patients that have spread to other places in general, liver, lungs, places like that, typically are not surgical candidates.
- You had mentioned Dr. Greenwald, that this is sort of...
I think the joke was it's this is a team sport here that there might be a lot of treatment steps if someone is treating gastric cancer.
Do you wanna talk about those?
Or, maybe... Dr. Oxenberg just brought it up.
- Yeah, Dr. Oxenberg, as she just mentioned to us, you need to evaluate the patient initially with... Usually they get a CAT scan, they get an endoscopy, and then they get the endoscopic ultrasound, which can tell you how deep it penetrates into the wall.
The endoscopist can see, and observe, and even biopsy lymph nodes next to the stomach.
They can often biopsy suspicious lesions in the left lobe of the liver.
And, so you get a lot of information.
And, then, as a group, you decide whether the patient, one, if it's a very early one, go right to surgery.
If it's more locally advanced, probably explore it or make sure that it's a surgical, and at that time decide whether you need pre-op radiation, and chemotherapy, and then surgery afterwards.
So, everybody is different and they don't all show up with the same stage and the same type.
- That's something Dr. Hanif mentioned actually a little bit earlier, that this is a very individual type cancer.
- It is.
Just like Dr. Oxenberg and Dr. Greenwald were saying, that it depends on where the tumor is coming from and what's the stage.
And, staging is probably the most important decision in developing a treatment plan for a stomach cancer.
The cancers that are closer to the esophageal junction, they are mostly treated with the incorporation of radiation.
But, the cancer that is strictly within the body of the... Of the stomach, we often do not utilize radiation for that, and we just utilize chemotherapy, followed by surgery, followed by some more chemotherapy.
So, it really depends on person to person.
Obviously, if the cancer is outside of the stomach, then you know that surgery or radiation have very limited role in that situation.
- This might be kind of a strange question, but if I... You break your arm, you go and get your arm taken care of, and you don't really have to worry, you have another arm and everything continues to work.
When it's your stomach you're talking about, you still have to eat, and drink, and you still have to function normally.
I wonder how that plays into treatment where you're now treating something that your body very much needs all day long.
Can you shed a little light on that for me?
- I think that's in Dr. Oxenberg's-- - That's the replumbing that I have to do.
- The replumbing, I like that.
- The replumbing.
Yeah, there's, depending on where the cancer is depends on what needs to be taken out.
But, believe it or not, the stomach, while it's nothing is as adequate as the stomach, the stomach is replaceable.
We reroute small bowel up to it.
If it's in the lower esophagus, we actually save some of this stomach and attach that to make a new esophagus.
So, it's...
Yes, you need it, but with a little bit of plumbing we can fix that.
- Sheer curiosity here, do you make that decision once you are there at the OR or do you know going in what the case might be?
- Almost all the time, we know what the case may be.
But, there are some times where, unfortunately, especially in some of the diffused types of cancers where we do have concerns in the operating room, whether it's one of the margins that we took out and pathology looked at it, or what it may look like, sometimes our plan may change.
So, a lot of it is going in and making sure that we do have all the workup beforehand and we know where the tumor is.
But, sometimes things do change if the margins are concerning.
- Somebody out there watching this just wants a little more information on this topic, what's the one message that you might really want to leave people with or, if somebody's watching, what do you want them to know most specifically?
- So, there has been tremendous improvement in all kinds of cancer in the last decade, but especially the stomach cancer.
There are newer treatments available, but those treatments might not be appropriate for everyone.
We decide the proper treatment based on the person's functional status, their general health conditions, and, most importantly, what kind of proteins are present on the surface of those cells, what kind of mutations are present in the DNA of the cancer cells.
And, based on that, we select the appropriate treatment.
So, I encourage everyone to do their research, but then bring their questions to their oncologist or they're treating physician and then discuss what treatment option is the best for them.
- What about you, Dr. Oxenberg?
- I just think, don't ignore your symptoms, but not every symptom is cancer, and I think that's probably, while gastric or stomach cancer is scary, it's rare.
There are people that are at risk.
We talked about genetic mutations, we talked about family history, but paying attention to your symptoms and knowing what your risk is I think is probably the most important thing.
- But, the vast majority of people watching this will probably not have to worry about this particular topic.
Vast majority anyways.
- Yes.
- Yeah, what about you, Dr. Greenwald?
- The vast majority doesn't have to worry, but if you feel you have something different, an inkling, start to lose weight, just don't hesitate.
Again, the endoscopy's an easy procedure, and don't be fearful, just get it done.
- Going forward, since it's not something that is typically screened for in a normal doctor's appointment, is there a... Are there questions that you would give to people to just talk to their regular doctor, or is there a plan of attack, or something that people should at least talk about with their doctor to determine whether they are at a high risk?
- So, if we know that if you have a family member with affected... Who is affected by stomach cancer, and that's a risk factor, sometimes there are syndromes that affect many different cancers.
For example, cancer of the stomach, esophagus, the colon, the pancreas.
They all come in as parts of certain syndromes.
So, if you have a strong family history of cancers in your family, do talk to your doctor about it, because you might be a candidate for genetic testing, and if a mutation is identified that does run through the family, that might warrant screening, screening endoscopies, to detect cancer before it spreads or before it turns into anything significant.
A general rule of a thumb is whatever symptoms you might have, if they're not improving with treatment or if they're growing worse with time, then that's a sign of concern.
- Is it that... Is it that it's not just stomach cancer then necessarily we're talking about here, but cancer overall, in other words.
It seems like a lot...
Some of the risk factors are the same for much of them.
Other than the location being in the stomach, is there any real difference?
- No, except, having done this for many years, it's...
I'm always shocked how people let obvious things go for so long.
People just don't lose 10 pounds, they lose 40 or 50 pounds.
They just don't have a mild back pain, but they can't get out of bed, and it goes over months.
And, I don't know if it's fear, and it could be, but too many people wanna put their heads in the sand, and not deal with things, because they have a high index of suspicion themselves.
They think that it could be and then they let it go until it's too late.
- I used to be one of those people 'til I started interviewing doctors.
I was the one who did not do any of this.
Dr. Oxenberg, what about you?
A final thought that you really want people to know?
- I think sometimes people, I feel like sometimes people put their head in the sand, 'cause they're afraid of knowing, but they're also afraid of the treatment, or what... What we have to offer.
But, gastric cancer is one of those types of cancers, there is some quality of life modifications, but if we can catch it early, I mean, it's treatable, and I do wish people wouldn't put their head in the sand.
- Okay, fine.
- Would see somebody after they lost 30 or 40 pounds, I wish they had came in at five, 10 pounds.
- Well, thank you to all of you.
It's been a great conversation.
I appreciate all of you and I appreciate you for watching.
That's gonna do it for this episode of "Call the Doctor".
We'll see you next time.
(uplifting music)
All About Stomach Cancer - Preview
Preview: S35 Ep2 | 30s | Watch Wednesday, February 8th at 7pm on WVIA TV (30s)
Clip: S35 Ep2 | 1m 15s | David Greenwald, M.D. - Medical Oncology Associates of Wyoming Valley (1m 15s)
Clip: S35 Ep2 | 1m 34s | Jacqueline C. Oxenberg, D.O. - Geisinger (1m 34s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorship
- Science and Nature

Explore scientific discoveries on television's most acclaimed science documentary series.

- Science and Nature

Capturing the splendor of the natural world, from the African plains to the Antarctic ice.












Support for PBS provided by:
Call The Doctor is a local public television program presented by WVIA