Call The Doctor
The Rise of Melanoma
Season 35 Episode 14 | 27m 4sVideo has Closed Captions
Dermatologists say they are finding more melanoma than ever before.
Melanoma is a type of skin cancer. The American Cancer Society calls it less common than other forms of skin cancer, but more likely to grow and even spread. Dermatologists say they are finding more melanoma than ever before. We wanted to make people aware of their sun exposure, of their moles and what role family history might play in diagnosing melanoma.
Problems playing video? | Closed Captioning Feedback
Problems playing video? | Closed Captioning Feedback
Call The Doctor is a local public television program presented by WVIA
Call The Doctor
The Rise of Melanoma
Season 35 Episode 14 | 27m 4sVideo has Closed Captions
Melanoma is a type of skin cancer. The American Cancer Society calls it less common than other forms of skin cancer, but more likely to grow and even spread. Dermatologists say they are finding more melanoma than ever before. We wanted to make people aware of their sun exposure, of their moles and what role family history might play in diagnosing melanoma.
Problems playing video? | Closed Captioning Feedback
How to Watch Call The Doctor
Call The Doctor is available to stream on pbs.org and the free PBS App, available on iPhone, Apple TV, Android TV, Android smartphones, Amazon Fire TV, Amazon Fire Tablet, Roku, Samsung Smart TV, and Vizio.
Providing Support for PBS.org
Learn Moreabout PBS online sponsorship(upbeat music) - [Announcer] The region's premier medical information program, "Call the Doctor."
- Melanoma is a specific type of skin cancer.
The American Cancer Society calls it less common than other forms of skin cancer, but unfortunately, more likely to grow and even spread.
Dermatologists say they're finding more melanoma than ever before and in younger patients than ever before.
We wanted to make people aware of their sun exposure, their moles, and what role family history might play in diagnosing it.
The rise of melanoma on this episode of "Call The Doctor."
Hello and welcome.
We are so glad you are with us for this season and this episode of "Call the Doctor."
We're talking about melanoma tonight, and we're gonna get right to the panelists.
We're really excited to welcome you all to the set here tonight.
I'd love if you could introduce yourself and let people know where to find you.
- Yeah, thank you.
Thank you for having me, I'm Dr. Ali Chittalia.
I work at Geisinger Internal Medicine in Mountain Top, and I'm also an informatician for the Steele Institute of Geisinger.
And I also work at the Graduate Medical Education taking care of the diversity, equity, and inclusion sense of it, yeah.
- Great, welcome back.
- Thank you.
- And hello, Doctor?
- Hi, my name is Lisa Thomas.
I am a hematologist oncologist at Hematology Oncology Associates of Northeastern Pennsylvania in Dunmore.
We are a group of six.
We all specialize in hematology oncology.
- All right, welcome.
- Thank you.
- And you, sir?
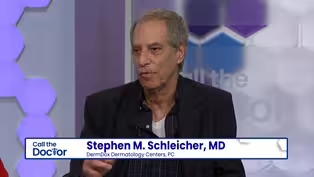
- I'm Stephen Schleicher.
I'm a board certified dermatologist.
I run DermDox Dermatology Centers.
We have eight offices, the closest one being Sugarloaf.
- Great, and welcome to you.
- Thank you.
I love that this panel is diverse in the different times you might see someone who has melanoma, so we'll use that to our advantage, I think, as we go through this panel, but first I kind of wanna start off with just the very, very basics that I think people confuse melanoma with skin cancer when one is a version of the other.
I guess we'll start with you.
Can you explain the difference there?
- So, there are different types of skin cancer, right?
One is a basal cell cancer, very common Squamous cells cancer is another very common type of cancer.
And melanoma is a type of cancer, but it is skin cancer.
It is not as common as basal and squamous cell cancer, but it occurs in the skin, in the melanin-producing cells when they get berserk and start to grow.
That is what we call a melanoma.
- Could you go into detail about the different types, Doctor?
- Well, yeah, I mean, basal cell is very, very common, okay.
Our president, his wife just had basal cells removed.
Reagan had basal cells removed when he was president.
Lots of basal cells, two million a year.
Melanomas are 100,000 a year, okay, so they're very less frequent, but they're far more deadly, okay, and that's why we're very concerned when we hear the word melanoma.
And of course, with oncologist here, she knows, you know, what melanoma can do, how it can spread.
- Is it that melanoma is skin cancer that has spread or it has a different shape, it's an entirely different kind?
- It's just a different organism, okay.
And most, you know, basal cells don't really spread internally, whereas melanomas, yes, they will kill you.
Okay, if you let it go, you'll die from melanoma.
- So, we'll, I guess, kind of get right into this.
What are some of the other differences between skin cancer and melanoma that you see, Doctor?
- So, melanoma is a type of skin cancer.
We talked about basal cell.
There's also squamous cell and melanoma.
So the hierarchy of how serious they are, basal cell being like we alluded to would be the least serious and doesn't metastasize, usually is treated by the dermatologist, local excision, and you're done.
Squamous cell, a little bit more complicated, may also need some additional treatment like radiation, doesn't need chemotherapy.
Melanoma is the more serious of the three, the most serious of the three, absolutely needs to be addressed surgically in multi-step procedures.
You also have to do lymph node sampling and plus or minus treatment depending on what stage it is.
- Are you seeing more of this?
Are you seeing more?
- Oh, we do see it.
So before we came on the air, we were talking about when I was in training at the University of Pittsburgh, there was a gentle by the name of John Kirkwood who was a melanoma specialist.
So you would rotate through his clinic, and we would see frequently melanomas, but if you even amongst...
Even today, melanoma is not that common, a cancer like breast cancer, colon, but it is absolutely on the rise, and it is definitely becoming a cancer of younger patients, particularly women because of their sunbathing practices.
- We're gonna get into that in a little bit here, but I would love to talk about what it looks like, who needs to be concerned and who does not need to be concerned?
So we'll start with you.
Do people come to you often and say, "Can you look at this?"
- Yes.
And so sometimes, you know, we find out when we are doing a clinical examination, a mole looks abnormal that somebody had, or there is a new mole that has sprouted, and we are taking a look at it, or we just find it incidentally looking for something else, abnormal skin lesion, which is pigmented or may not even be pigmented.
And sometimes the patients find it themselves, or one of their, you know, family member or close spouse will take a look and say, "This doesn't look right.
"Go get checked out."
And then they come to us.
But anytime when a patient shows concern about a skin lesion, we, as you know, internists, primary doctors, primary care, we have to take it seriously.
- And it seems like a...
I mean, I'm not putting words in your mouth.
This is a fairly easy one.
Like, you can come to the office, I take a look at your skin.
- Yeah, it can.
And the incidence of melanoma is rising.
It is the fifth most prevalent cancer in America.
- So Dr. Schleicher.
Actually, any family occasion, 50 million people come up to you, "What's this, what's this, what's this?"
(panelists laugh) Okay, so, it's like never fails, right?
- [Julie] You're the one they call.
- Go on a curbside consult.
- [Julie] Do they send you cell phone pictures of their moles?
- Of course.
- Oh, absolutely, absolutely.
- Of course, yes, yes, yeah.
- Well, can you tell people who are watching then what to look for?
I know the ABCDE came up in some research, but what are we looking for?
- Right, so you're looking for, first of all, any mole that changes, okay.
You wanna be very, very careful about a mole in which one side doesn't look like the other side.
We say asymmetrical.
Okay, that's a bad sign.
Border, if the mall has notching, okay, If it's not totally even around, that's a bad sign.
Coloration, well, everybody knows dark is probably not really good, but there's certain other colors.
Very easy to remember, red, whites, and blues.
If you see that in a mole, that's a very, very bad sign too.
D is for diameter.
We talk about the ABCDEs of melanoma recognition.
It's a general rule if you can put a pencil eraser over the mole and can't see the mole, chances are it's not too serious.
And E stands for evolving or elevation.
Any mole that's kind of changing.
Again, you wanna bring it to someone's attention, but there's a very important sign.
It's called the ugly duckling sign, okay, because you have people with...
Some people can have 20, 30, 40 moles, but if you look and there's one that just really looks odd, that's the ugly duckling, and that's not good.
You want to get that checked out, for sure.
- Some people are just molier than others for lack of a better term.
Are they at a higher risk if they have more moles?
There's just at an increased risk of one of those moles not being totally- - The more moles you have, the greater the chance that one is going to change.
Okay, so that's true, absolutely.
- What are some of the things that you have seen?
And, again, I use anecdotally, but what are...
I guess a better question is, do people come to you in time, or do you often see them when they're perhaps a little far gone?
- So I've seen melanomas with ulcerations and bleedings, and some of those melanomas have already gone somewhere, you know, metastasized or gone internally.
I've had two patients like that.
I had a patient that I saw with melanoma in the scalp that we were lucky enough to find it because it just... And it looked like something like a keratotic lesion, which is like a thickened skin.
It did not look very suspicious.
But somehow or the other, I wasn't too comfortable letting it go.
So we called a dermatologist.
And the key for us, and especially in primary care, is when you find something that looks abnormal and you have a risk for melanoma, pick up the phone and call the dermatologist, you know, that, hey, I want this person in.
I don't want... Because, you know, there are few dermatologists around, right?
The waiting time is large, and you don't want people to wait months to get attention for that lesion.
- I think you bring up a very important point with the scalp melanoma because we encourage hairdressers.
I mean, most people can't see their scalp, okay, and even their back.
So who's gonna find it, okay, especially in the scalp?
A hairdresser.
So they may be the first person to... Could save your life by getting a haircut.
So that's a side benefit.
- I never even thought of that that that would be something that they would have a perspective on that no one else would.
- Absolutely.
- When we talk about it metastasizing, where could it go?
- So why don't you bring up one point, you know, I do agree melanoma is very serious, but melanoma is a completely preventable bad actor, okay.
So, you know, I think I was saying this before is a lot of times you can't see cancer.
You can't see colon cancer.
You may feel like something's a matter, but you can't see breast cancer, but in 75% of the time, you can see melanoma because it's obvious on the skin surfaces.
There are melanomas called hidden melanomas, which is important to discuss because those are ones that really do hide.
They're under the nail bed or they're in the intestinal tract.
They're not obvious melanomas that are associated with UV exposure.
- [Julie] What does it look like under the nail bed?
- It looks like it actually...
It's mistaken a lot for...
It looks like somebody who bangs their hand with a hammer, their nail bed with a hammer.
- Or could look just like a streak.
- Or just like a streak.
- A banded streak.
- Like someone just hit it or something.
- Not even that, it's just a line.
- Just a line, and people, they'll think that they just traumatized it, so they'll wait until it grows out, and it doesn't grow out.
And so you do have to be cognizant of the hidden melanomas as they're called.
- And what did you say, intestinal melanoma?
- There's intestinal melanoma.
There's a very common one is ocular melanoma where people can get melanomas behind their eyes, and usually they present with visual changes, and they're diagnosed by an ophthalmologist as opposed to one of us.
So there are melanomas that are not the usual type that we think about.
- But the majority, you can see, which is a good thing, okay, which is real good thing.
- Well, you would think that if you can see them, they would be diagnosed very early.
So I guess I wonder why people- - Well, you would hope so, okay, but people just neglect things, or they don't see them, okay, or I mean, you mentioned your training.
A lot of family practice residents have no derm training.
Okay, so even doctors don't know sometimes which mole could be bad or which mole isn't.
And like you said with the shortage of dermatologists to get in to see them, it might take months.
- Yeah, I have a very low threshold for those pigmented-looking lesions that are irregular and, you know, asymmetrical, or sometimes they look literally like nodules.
There's a type of melanoma, which is like a nodular melanoma, which it just doesn't even have the dark pigmentation.
It might just look like a pink bump.
And those kind of areas you have to be careful about.
Also melanomas on the foot that acral lentiginous melanoma, which are on the sole of the foot and the palms, I mean, the palm, you can look at the lesion and think that there is something going, but nobody really looks at the soles literally - Your feet.
- Until they're looking for something, right?
- And you bring up a good point again because blacks by and large don't get skin cancers, but they do get melanoma.
And where do they get 'em?
On the palms, okay, the soles and the nails, and that's very, very neglected because people, you know, you have black skin?
Well, you can't have skin cancer.
Bob Marley died of a melanoma, okay, of his toe.
So we have to be very, very careful of the Hispanic, black, but darker-skinned patients because they get melanomas sometimes in different areas.
- Yeah, usually it is a condition seen in lighter, fair-skinned people, you know, red hair, blonde hair, light colored eyes.
That's a typical... You know, like if you wanna stereotype it, that's the type of, you know, patients that you see it, but melanoma is on the rise.
I don't know if you guys think is it better because there's better detection techniques, more awareness, or is it truly a rising incidence?
- Well, that's a great question.
There's rising incidents because of why?
Indoor tanning.
All right, so we go berserk.
I mean, I yell at patients all the time because somebody who has fair skin, every time that person goes in a tanning booth is increasing their risk of skin cancer like immeasurably.
Okay, so you're not doing yourself any favors by going into a... And so many college kids do it.
Teenagers do it.
It's really horrendous.
- But to Dr. Thomas's point earlier on, it's not necessarily what you're doing now, but the damage that was done how many years ago, and that is a good how many years ago?
- Well, that's another great point because we see kids who are totally out in the sun without hats, without, you know, proper clothing, without sunscreen.
And the more incidents you have of sunburn as a kid, the greater the chance you're gonna get melanoma as an adult.
- I do think, though, that public awareness is much better than it was.
Like when I think when I was growing up, we didn't do those things.
Okay, we were always in the sun, and, you know, I was vigilant with my kids, right, about putting sunscreen on them and clothing and protecting them.
So I think public the awareness is really been beneficial to melanoma.
I do think that people do neglect things, and especially if you have a lot of moles, you know, it's hard to single out until it gets to the point where it's obvious.
It starts to bleed.
There's certain things that sort of clue you in that there's a problem, but, you know, a flat lesion that maybe looks a little bit irregular can still be an early melanoma.
There's a thing called melanoma in situ, which is a pre melanoma condition.
Those are when you have to find it and treat it.
So I always say to patients, you know, there's no harm in taking a skin lesion off, right?
If it's not a melanoma, if it's not a cancer, then okay, it's not, but if it is, then we've discovered it early.
Just like with any other cancer, early detection leads to better prognosis.
- And you bring up a good point too because people with 20, 30, 40 moles, you're not gonna take every mole off, but we have an instrument in the office called a dermatoscope, and we can actually magnify, almost look under the skin.
So we can go through mole after mole after mole within 30, 40 seconds and see which ones are kind of suspicious that you would never tell what you're naked eye.
And so you're not gonna biopsy every mole and have little scars on, you know, patients.
Not going to happen.
- Let's go back to the question I asked earlier about if the cancer has spread, are there common areas for it to go?
Can it be anywhere in the body?
- Melanoma is very systematic when it's spreads.
So there are a few malignancies that are like that.
Melanoma's one of them.
So melanoma tends to go to the lymph node first that's near it.
So that's called a sentinel lymph node.
So part of the treatment process for melanoma is to biopsy the melanoma, to remove the melanoma with an area around it that's called a white excision.
So you're taking off skin that's not involved to make sure that you don't leave behind any melanoma.
And then the surgeon will do what's called a sentinel node mapping, and that's using a radioactive tracer to light up the node that could potentially drain the melanoma bed.
So to make it clear where you remove the melanoma, if I take it off my hand, that's the melanoma bed.
That area, even without melanoma, may drain to my arm.
So what the surgeon does is they take off the melanoma, and then they use a special tracer and they isolate a node, and if it lights up, that's called a sentinel node.
They will remove that node and they will test it for melanoma.
So melanoma is not something that usually goes from, say, the hand to the liver or the hand to the lung.
It will go to from the hand to the lymph node and then start to spread to other places, and it can go anywhere just like any cancer.
It can go to the liver.
It can go to the lungs.
It can go to the brain.
It can go to lymph nodes and other parts of the body.
- And just to clarify, most people with melanomas don't need that sentinel node biopsy.
It really depends on the depth of the lesion, which all the viewers, okay, the earlier you catch this, you can cure it.
It's curable, okay, but you see that, you know, the depth is too great, those are the people, yeah, we send for that sentinel node biopsy.
- So just to clarify, what he is talking about is called a Breslow depth.
So when you stage melanoma, you stage it based on the depth of invasion.
So that means the skin is the top.
How far does it go into the area below the skin?
And it's measured in millimeters.
So they'll say a Breslow level of two millimeters, and that, as well as the lymph node, the size of it will all fit you into a stage, and there's a stage one through stage four.
And so the Breslow thickness is how far below the skin, and that's part of the staging for melanoma.
- And you'd all mentioned that family, hereditary.
- Absolutely.
- There's a component there.
- There is.
There's a component of family history.
If families have parents have had it, or if they're two first degree relatives, there's a much higher chance of having melanoma.
There are certain genetic mutations that some patients may carry that predisposes them to risk factors.
Immunocompromised status, you know, people who have lower immunity are at a higher risk, but let's talk a little bit about not having to go to see Dr. Schleicher or Dr. Thomas.
Like prevention is what I strongly recommend.
Summer is coming.
We must talk about like sunscreens using those UV ray protections at a higher SPF of 30 at least if needed in darker skin people, or if you burn a lot, you have high level of, you know, propensity of skin burns, then use a 50 SPF.
And if you're going swimming, maybe use it every couple of hours.
You know, that really prevents skin damage and induction of them small lesions turning into cancer or new lesions developing like melanoma.
So prevention, I agree with you there.
- And start early too.
Start with your kids because you really wanna get a good habit going, okay, because some people just don't think.
People still worship the sun.
And as you said, the higher the sunscreen, usually the better, okay?
So people ask us all the time, "What numbers should I use?"
Well, I mean, 15's about the lowest.
Well, it is the lowest you can get, but if you can get a 50, if you can get a 70, now they're more expensive, but they offer an awful lot more protection.
- I'm interested in the role that your immune system plays.
I guess I hadn't really thought much about this until we discussed it earlier.
We were talking about immunotherapy, which led us to talk about kind of revving up your own engine, so to speak, to be able to fight whatever invader.
Could you talk a little bit about that?
I probably didn't make much sense there in that context.
- No, you did, you did.
You actually did.
So, cancers, when you talk about treatment for cancer, there's chemotherapy, and then there's biologic therapy or immune therapies.
They're the hottest, newest thing, right?
So chemotherapy, to make it simple, is just the drug that you give goes to the cancer cell and makes the cancer cell go away.
Melanoma is not treated anymore.
It used to be treated with chemotherapy.
Now it's treated with what's called immunotherapy.
It's very dependent on how you could rev up your own immune system.
So just like we talked about immunocompromised patients having increased risk, HIV patients, patients who have had organ transplants who are on drugs, their risk for skin cancers increase.
The exact opposite, what we wanna do is we want to increase the immune system to help your own body to fight melanoma.
So the therapies for melanoma, when we talk about... And I'm sure we've all seen the commercial for Opdivo and Keytruda and those things, those are biologic therapies.
They're called checkpoint inhibitors, and what they do is they don't go to the melanoma cell and kill the cell directly.
They go to your immune system and they turn on your immune system to go and fight the cancer.
So they're so successful.
Not all cancers can be treated with those, but they are... Or you could use what's called targeted therapies.
So certain melanomas have mutations, which are very common.
One is called BRAF.
There's MEK mutation, CKIT mutations.
So there are actually drugs that can target those mutations if they're present in the cancer cell, and by attaching to the receptor in the cancer cell can make the cancer cell go away.
- And what we had talked about earlier too, I mean, melanoma that spread used to be a death sentence.
- [Lisa] Death sentence.
- I mean, you look at the patient and you say to yourself, "This patient's gonna be dead in six months."
And now we're getting patients with metastatic spread who are alive, you know, 10 years- - Without disease.
- Yeah, yeah, which is fantastic.
- Can you be on those drugs long-term?
- You can be on some of them, you can.
So the oral ones, the targeted therapies, you can treat for longer periods of time.
The biologic therapies like Keytruda and those things, they cause autoimmune because we're working on the immune system, so they can have autoimmune side effects.
So generally, if you're treating metastatic disease and you get somebody into a remission or quasi remission, you can treat for two to three years, barring no side effects happening.
- And what might some of the side effects be?
- So the biggest side effects, some of them are you just treat through them.
So what they do is they create autoimmune disorders.
So one thing would be like a thyroid disease.
So patients may have to be put on thyroid medication.
They can develop colitis.
So you may have to treat them with steroids.
So a lot of the stuff you can treat by just adding a medication.
If the side effects are severe like somebody has intractable GI side effects, if they develop inflammation of the liver called hepatitis, then the drugs have to be stopped, the dose reduce or stopped.
So, the patients actually monitored very carefully.
And sometimes we use those drugs when they've taken off a melanoma to prevent it from coming back like a high-risk melanoma that, say, spread to a lymph node.
The patient will have surgery, they'll be without evidence of disease, we'll treat them to keep it away.
Other times we treat them to try to take it away.
So there's two different approaches.
- And it would be just dependent on that particular patient, that particular case?
- What stage they have.
That's correct.
- Some patients who have genetic mutations, I as an internist need to figure out, there's some patient who has a melanoma with underlying different genetic mutation, then I have to make sure that the patient is getting screened for other cancers that they are more predisposed to like pancreatic cancers and kidney cancer.
So just managing the melanoma and not looking at patient as a whole would be disservice.
- And not only that, it's getting the whole family involved because if it's genetic, some people don't even realize it.
So we've gotta contact family members and let them know and, you know, because they're at risk too.
- Well, even one of the more common skin cancers that you mentioned earlier that you see a lot, the two million or so I believe was the number you gave per year, if someone has one of those, are they at a higher risk?
Are they gonna be monitored differently than the general population?
- Well, most basal cells are so- - They're so common.
- Yeah, they're very common.
They're very benign, and 99.9% of them never metastasized to your lung, to your lymph nodes.
They'll just get bigger.
So the problem we have is getting rid of 'em surgically, but we don't really worry about them going internally.
So it's a whole different ballgame.
It's a whole different type of cancer.
- But the same risk after for basal cell and squamous cell are for melanoma.
So it's sun exposure, immunosuppression.
So patients who have had one of those, even if you have had a basal cell, you would counsel them.
This isn't gonna go anywhere else.
However, your risk of getting another basal cell is very high, and your risk of getting another type of skin cancer, I've seen that too where they get a squamous cell or melanoma.
So they do have to be followed more carefully.
- Well, I hope if nothing else, we have at least gotten someone to check themselves out or have a loved one check out, you know, what their moles might look like.
Screening seems to be... Maybe screening isn't the right word, but letting your doctor know that you have a family history and letting them check you out seems to be the best way to go.
- And there are screening programs.
So the NRCI in Scranton, there are institutions that offer free screenings.
So you could show up and, you know, if you think something... You know, sometimes they're not doctors, but here's the thing, like I said, if they take off a mole and it's not a melanoma, it's okay.
- Right, it doesn't matter.
- If there's an ugly lesion that you are concerned about, don't let it go.
Don't sit on it, don't wait.
It's not going to disappear.
- Text him a picture of it.
- Yeah.
(all laugh) - Yeah, right.
He'll be one of the doctors calling me.
(all laugh) "Can you get this patient in like really quickly?"
- And we at Geisinger, I'm gonna tell you something quick, we have a great service that I can do an electronic consult.
I can send a picture to my dermatologist, and they can take a look at it quickly and let me know, hey, this one needs to be seen in the clinic.
If I'm not sure what's going on, I will reach out right away.
- I hope at least we've gotten through to someone.
I wish I could keep you here for longer, but thank you all for your expertise tonight.
We very much appreciate you.
- Thank you.
- That's gonna do it for this episode of "Call the Doctor."
We're so glad you've joined us.
You are welcome to watch this over.
If you missed something, you wanna listen to it again, you can see the whole show at our website, wvia.org.
For all of us here at WVIA, I'm Julie Sidoni.
We'll see you next time.
(upbeat music)
Aliasgar Z. Chittalia, MD, MHA
Clip: S35 Ep14 | 41s | Aliasgar Z. Chittalia, MD, MHA - Geisinger (41s)
Clip: S35 Ep14 | 43s | Lisa C. Thomas, MD - Hematology & Oncology Associates of NEPA (43s)
The Rise of Melanoma - Preview
Preview: S35 Ep14 | 30s | Watch Wednesday, May 3rd at 7pm on WVIA TV (30s)
Clip: S35 Ep14 | 1m 9s | Stephen M. Schleicher, MD - DermDox Dermatology Centers, PC (1m 9s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorship
- Science and Nature

Explore scientific discoveries on television's most acclaimed science documentary series.

- Science and Nature

Capturing the splendor of the natural world, from the African plains to the Antarctic ice.












Support for PBS provided by:
Call The Doctor is a local public television program presented by WVIA